AFP is short for Alpha FetoProtein.
As the “feto” in the name suggests this is a protein we see in a fetus. In adults we switch off the genes that produce it so we don’t see much (usually <12 units)
Hepatocellular Carcinoma (HCC) represents a loss of control over liver cell growth. These liver cells tend to become more primitive, like the liver cells in a fetus. What often happens is that the genes that produce AFP get switched on again, so instead of seeing <12 units of AFP we see more.
In pragmatic terms:
Most patients will have an AFP <12 and will not have HCC
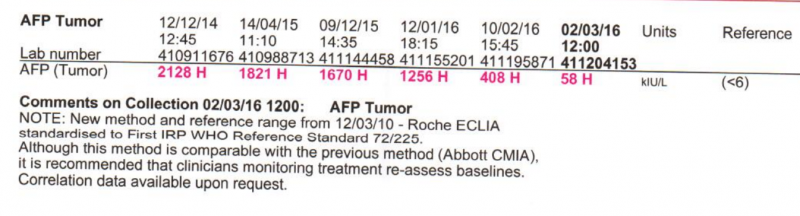
Some cirrhotic patients will have a slightly elevated AFP in the range 12-24, despite not having HCC. We invariably see this fall during and after treatment. Sitting on my desk I have these results from a cirrhotic patient who is now at SVR
Most, but not all, patients who develop HCC will have a detectable rise of AFP, usually to a level of over 100
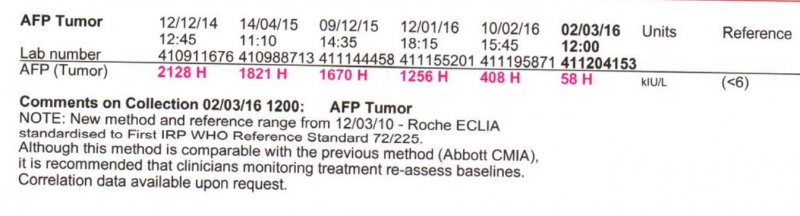
Here is a patient who had HCC in whom we treated the HCV and the HCC (with Sorafanib). Notice both the fall in AFP and the fact this lab uses <6 rather than <12 as the cutoff
Please note this: while most HCC expresses AFP and therefore can be detected by an AFP blood test it is possible to have HCC with a normal AFP. Rare but possible. High risk patients with cirrhosis should have 6 monthly screening with U/S (or CT or MRI)
Also note that if you have had HCV but have not developed cirrhosis then your risk of HCC is almost exactly the same as the general population. It happens, but it is rare. AFP screening is more than adequate. If you want to have a look use U/S or MRI as a CT carries about a 1:1000 risk of giving you a cancer (it might be a little lower than this but is does carry a real risk).