Forum Replies Created
-
AuthorPosts
-
What medication are you taking?
YMMV
Hi Tanya,
There are many causes for feeling unwell and having elevated liver functions, but in somebody who has just finished treatment for hep c with Zepatier (or Harvoni or Maviret or Epclusa) treatment failure would be top of the list.
While the treatment failure rates are low 95% cure rate means 5% failure rate – so if I treat 20 patients with Hep C this week one will fail.
As Mar has said – you need an HCV PCR RNA test to see if the virus is still present.
If it is, don’t panic. Retreatment is easily done and very effective.
If it isn’t we need to look for other causes of problems.
Either way you probably need a doctor with more of a clue…
YMMV
Hello Oregondaisy,
You’re unusual in your supplements in that many of them (not all) have potential benefits or are clinically relevant to you.
Vitamin deficiency following sleeve gastrectomy is known so continuing your vitamins is both a good idea and won’t impact treatment. A mutli B (not just B12) and vitamin D are best.
Nutritional Deficiency After Sleeve Gastrectomy: A Comprehensive Literature Review
Milk thistle contains silymarin and there is some evidence it may help untreated patients
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4076489/
But, there is also some evidence it does not do anything much
https://nccih.nih.gov/research/results/spotlight/071812
While I suspect it should not interact, the best treatment for HCV related liver disease is to get rid of the HCV so stopping milk thistle during treatment avoids any worry of interaction. The major benefits are flowing from the DAAs. You can continue it after, but after treatment, you’ll find your liver enzymes are normal and you can’t get better than that – the cause is gone so…
In general, as far as your body is concerned, collagen and gelatin are just different forms of protein. They will be digested in your gut into their constituent amino acids and from there do no more, no less than eating a little chicken, red meat or fish. I’d rather have the real food myself, it’s tastier and more natural.
That said, undenatured type II collagen (UC-II) is not intended to be used by your body as a collagen re-builder. In a process called oral tolerance, very small doses of UC-II are taken to train your body’s immune system to stop attacking its own collagen
Here is a vox pop on it:
http://blog.arthritis.org/living-with-arthritis/collagen-supplements-helpful-arthritis/
And here is a medical literature review suggesting a net benefit:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4970562/
So UC-II in low dose would be a probable yes. It should not interact with DAAs.
With Chondroitin/Glucosamine there is some weak evidence they may help. I certainly have patients who say they benefit. Here is a review:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5241539/
So I’d suggest that while on the treatment:
- You should take the B complex + Vitamin D and it won’t interact.
- I’d skip the Milk Thistle for now and don’t think there is going to be a reason for it after.
- General collagen and gelatin are no better than fish/meat based food which is natural and tastier.
- UC-II collagen at low dose may be useful and won’t interact.
- The chondoitin/glucosamine are fine to continue, probably beneficial and won’t interact.
YMMV
Hello Oregondaisy,
Yes, supplements don’t appear on most interaction charts because it’s impossible to know what’s in most of them and what doses people are taking. There is no doubt that some will interact, and some won’t but we don’t know which ones.
On the general topic it’s probably worth reading this:
More evidence that routine multivitamin use should be avoided
While it’s not true that 100% of supplements are 100% useless, it is basically true they represent 90% marketing on top of 10% fact – more hope than evidence if you like.
Most patients, taking most supplements, are either no better off, or actually worse off because of them.
There are exceptions, but most people need no more than clean air to breathe, clean water to drink, personal hygiene, and a good varied diet to eat to live a long and healthy life.
If you’d like to list your supplements and what benefits you expect from them, we can have a discussion about the pros and cons of each.
YMMV
This is not the same company but is cheaper and has a free and immediate test/trial
YMMV
18 January 2019 at 6:32 am in reply to: Proton Pump Inhibitors Linked to Advanced Liver Disease in Hep C #28926Hi John,
Here is the original article (abstract): https://onlinelibrary.wiley.com/doi/abs/10.1111/apt.14391
And here is an editorial talking about it: https://onlinelibrary.wiley.com/doi/full/10.1111/apt.14431
So if you read this:
Background: Proton pump inhibitors are among the most commonly prescribed medications in the United States. Their safety in cirrhosis has recently been questioned, but their overall effect on disease progression in noncirrhotic patients with chronic liver disease remains unclear. Aim: To determine the impact of proton pump inhibitors on the progression of liver disease in noncirrhotic patients with hepatitis C virus (HCV) infection. Methods: Using the electronically retrieved cohort of HCV-infected veterans (ERCHIVES) database, we identified all subjects who received HCV treatment and all incident cases of cirrhosis, hepatic decompensation and hepatocellular carcinoma. Proton pump inhibitor use was measured using cumulative defined daily dose. Multivariate Cox regression analysis was performed after adjusting univariate predictors of cirrhosis and various indications for proton pump inhibitor use. Results: Among 11 526 eligible individuals, we found that exposure to proton pump inhibitors was independently associated with an increased risk of developing cirrhosis (hazard ratio: 1.32; 95% confidence interval: 1.17-1.49). This association remained robust to sensitivity analysis in which only patients who achieved sustained virologic response were analysed as well as analysis excluding those with alcohol abuse/dependence. Proton pump inhibitor exposure was also independently associated with an increased risk of hepatic decompensation (HR: 3.79; 95% confidence interval: 2.58-5.57) and hepatocellular carcinoma (HR: 2.01; 95% confidence interval: 1.50-2.70). Conclusions: In patients with chronic HCV infection, increasing proton pump inhibitor use is associated with a dose-dependent risk of progression of chronic liver disease to cirrhosis, as well as an increased risk of hepatic decompensation and hepatocellular carcinoma.
Then you’d be correct that there appears to be a risk but it needs to be taken in context. With the cirrhosis risk of 1.32 we have a 95% confidence interval of 1.17 to 1.49 which means we think there is a 17% to 49% increase in cirrhosis risk (and are 95% sure it’s in that range). So that’s an increase in cirrhosis risk, but the biggest risk for cirrhosis in HCV is HCV so if you get SVR then your general risk profile changes like this:
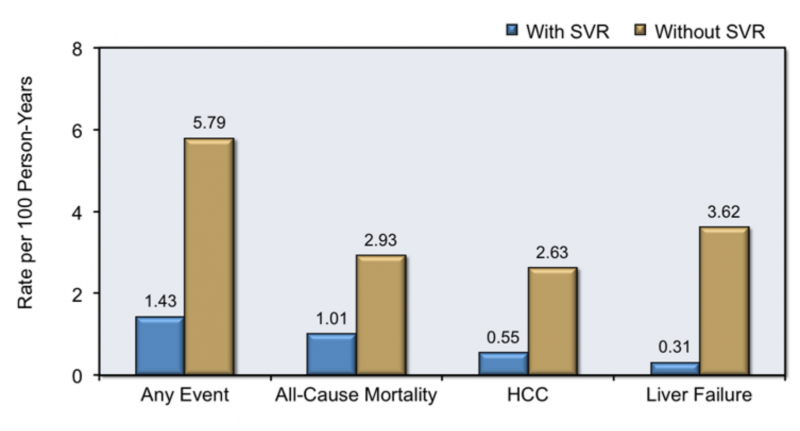
So SVR delivers 1/3 the rate of mortality, 1/5 the rate of HCC and 1/10 the rate of HCC.
It looks like PPIs may compromise that improvement slightly. From memory, your 2 major issues were the HCV (now cured) and being overweight (substantially increasing the probability of fatty liver) and which you’re working on. These are the big ticket health issues, and your reflux would almost certainly be improved by weight loss allowing you to use less PPIs.
So, in terms of long term health look after the big ticket items first.
- Get rid of diseases like HCV and try to be in the healthy weight range
- Get your blood pressure, cholesterol and blood sugar checked and fix if needs be
- Don’t smoke or drink too much alcohol
- Do exercise, eat good food, drink water and get enough sleep
Once you have the basics to hand look at the smaller issues like PPIs. There is no such thing as a drug that does not have side effects and you don’t get any issues with drugs you’re not taking. This advice also applies to supplements, most of which have been shown to have no long term benefits and some long term issues.
YMMV
Hi John,
Thanks for the kind words. Here is a cryptic clue…
As Mar says we are 99.7% certain you’re cured so it’s fair to say the fat lady is definitely warming up.
In another 8 weeks (SVR24) undetected is cure. At the moment it is >300:1 in your favour.
YMMV
Hi Boba,
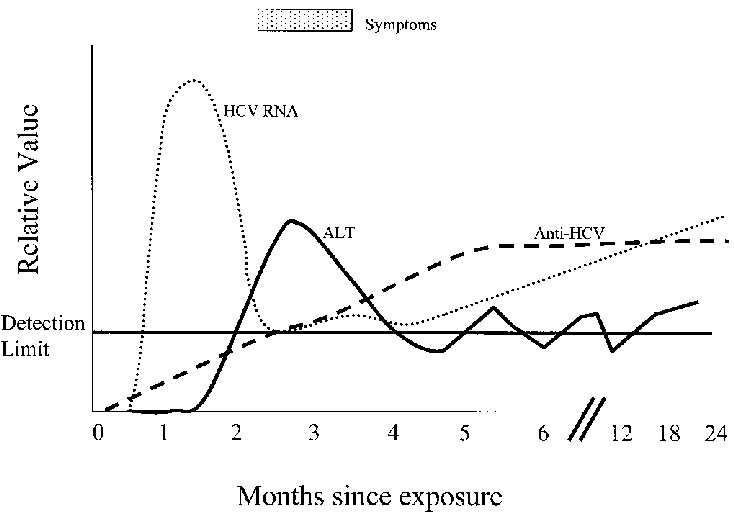
If you have a look at the first graph you see an early spike of HCV RNA – this is the viral load. It peaks and then the partially (for some people fully) effective antibodies start to rise and knock it down.
Either the antibodies wipe it out or the vius mutates a bit and starts to go up again. It’s all normal and your treatment success probability is very high.
Trust in the force young Jedi!
YMMV
Hello Boba,
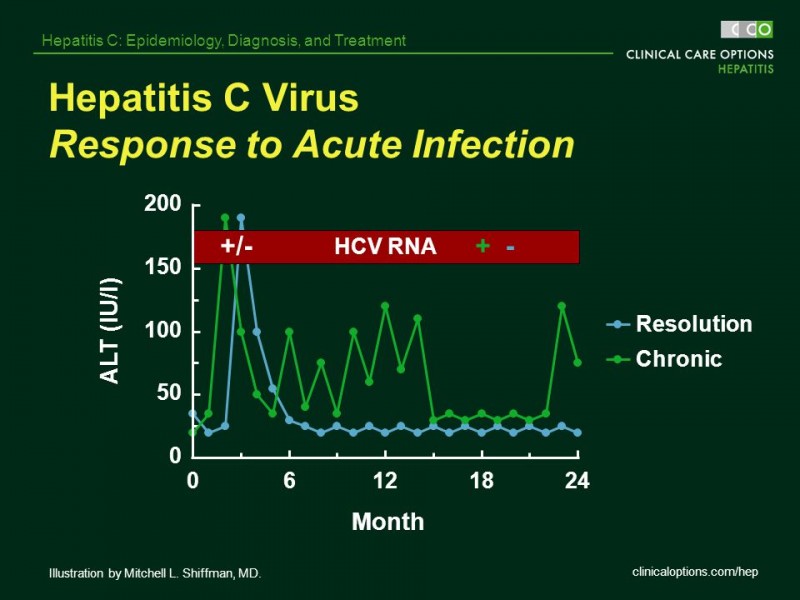
It’s normal for both ALT and Viral load to fluctuate during the acute phase. It looks roughly like this:
About 25% of patients clear the virus and you can see the comparison here where one patient clears the virus and the other patient does not:
Dual genotypes probably occur ~ 10% of the time but are less often reported. Over time, whatever genotype reproduces fastest will become the dominant one, so in your case, it looks like the GT2 more or less beat the GT1a in the cloning stakes.
Epclusa works on both GT1a and GT2 (and all the other genotypes) so your cure rate is not better/worse because of this.
Early treatment tends to be more effective than later treatment as there has not been time for cirrhosis to develop and we know this makes treatment harder. It’s probably only a 2% chance (1 in 50) that you won’t clear on 12 weeks of Epclusa. While it’s nice to see undetected on treatment if your ALT/AST are good, then things are going well. Once you finish the pills they wash out in a week, giving the virus 11 weeks to grow back (if still present) which is why we wait until SVR12 – 12 weeks after the pills finish – to declare cure (it’s 99.7% certain you will remain negative indefinitely if negative at SVR12).
YMMV
Hello Penn,
There is quiet a strong association between autoimmunity and Hepatitis C. The immune-related extrahepatic manifestations include:
- Mixed cryoglobulinemia
- Cryoglobulinemic vasculitis
- B-cell non-Hodgkin’s lymphoma.
- Sicca syndrome
- Arthralgia/myalgia
- Polyarthritis/fibromyalgia
- Autoantibody production (i.e. cryoglobulins, rheumatoid factor, and antinuclear, anticardiolipin, antithyroid and anti-smooth muscle antibodies)
- Polyarteritis nodosa
- Monoclonal gammopathies
- Immune thrombocytopenia
- Glomerulonephritis and renal insufficiency
This article speaks to your questions https://rmdopen.bmj.com/content/1/1/e000008 with the answer “we just don’t know”.
This article says “use DMARDs with caution in HCV” http://www.eurjrheumatol.org/sayilar/211/buyuk/194-9.pdf
This article suggests slightly lower SVR rates in patients with autoimmunity https://bmjopengastro.bmj.com/content/5/1/e000203
There is a tiny 3 case series here https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-018-0826-7 showing a transient fall in autoantibodies during treatment
But in terms of a study that said something like “patients with HCV and autoimmunity have reduced autoimmunity on and after HCV treatment” – as far as I know nobody has done a large trial to answer that one way or another.
It sounds like you are weighing up treatment options?
YMMV
If you ALT is continuing to fall, and platelets continuing to rise… you will be fine. The PCR will be negative.
YMMV
Hello Aaron,
The cure rate for GT2 with either Sofosbuvir/Daclatasvir or Sofosbuvir/Velpatasvir (Epclusa) is very high. Not quite 100% but close.
The 12 weeks of waiting is hard. You can check your liver enzymes every 4 weeks and if these remain normal you can be confident that all is well. A CMP from link2labs https://fixhepc.com/link2labs will cost $10 so it’s a cheap way of keeping tabs on things.
Best of luck, but, if you were a horse, I’d be betting on you for the win.
YMMV
Hi Chris,
I’ve sent you an email about making a quick appointment so we can discuss it.
If it was me I would have started with it, and would add it now regardless. While 22% of people are still detected at the 4 week test, and these people form 44% of the failures, 56% of people of the failures come from people who are undetected, so while being undetected is better than being detected it does not really help that much. If you were still detected definitely add riba, if undetected I’d still be feel happier if you were taking it.
Ribavirin has significant side effects (compared to Epclusa alone) although you will barely get to them taking 8 weeks. It’s not as bad as when mixed with PEG Interferon, and some people tolerate it very well. It’s about 1/3, 1/3, 1/3 between not too bad, not great and awful in terms of patient experience.
The irritability aka “Riba Rage” is a problem in some people.
YMMV
Hello RockHard,
11.6kPa is less than the 12.5kPa for cirrhosis but, given this is a spectrum you are much closer to cirrhosis than not. As you say, for F4 GT3 patients the recommendations are 12 weeks Epclusa with Ribavirin or 24 weeks without.
If you were my patient I would have discussed this in a conversation like GT3 is harder to treat, it’s harder with cirrhosis (which you are close to) so what do you think about Ribavirin?
What country are you in? There are all sorts of rules that restrict what can be used and the options for retreatment also vary. For example, in Australia all I could give you would be 12 weeks Epclusa so the decision here is 12 weeks with Riba or 12 weeks without – there is no 24 week without option. For a patient in Australia, the only way to do 24 weeks without would be 12 weeks PBS funded, and 12 weeks self-funded generic.
All other things being equal I would be happier if undetected at 4 weeks than if you’re still detected.
Yes we could add Ribavirin in later. It’s probably not as good as earlier, but probably better than not at all. The “probablys” relate to the fact it’s not done very often so it’s a best guess, rather than something backed by solid research. I know eminent doctors like Professor Ed Gane would add it in if things did not seem to be going according to plan (at least that’s what he suggested last time I asked!).
YMMV
29 December 2018 at 8:50 am in reply to: I take Protonix and it interacts with Harvoni. What to do? #28879Hello OregonDaisy,
The peak of the effect of the Protonix is about 1-2 hours after taking it. After that the blood levels fall and the acid starts to return. So, your stomach is most acidic more or less the moment you take the next dose.
By taking the Harvoni 1 hour before, you give it the most acidic environment possible, and what amounts to a 1 hour “head-start” on the effect of the Protonix.
This is what happens to stomach acidity over the course of the day with twice daily dosing of a PPI.
You may notice that meals see the pH of the stomach reliably rise.
Anyway what we should do it make a time to have a chat about using Daclatasvir, make sure there is nothing else you are taking that might cause issues, and then make a plan.
YMMV
-
AuthorPosts
