Forum Replies Created
-
AuthorPosts
-
28 December 2018 at 6:20 am in reply to: I take Protonix and it interacts with Harvoni. What to do? #28872
Hello Oregondaisy,
If you must take Protonix it should be the lowest dose possible and taken only in the morning about 1 hour after the Harvoni.
It would be better for you to take Sofosbuvir + Daclatasvir rather than Harvoni as the absorption of Daclatasvir is not impacted by antacids (unlike the Ledipasvir in Harvoni).
It is unusual, but possible to add Daclatasvir to Harvoni to deal with this problem.
YMMV
At SVR24 we are 99.99% certain there will be no relapse. The 1:10,000 who do relapse are suspected to be reinfections, rather than true late relapse cases.
This makes sense when you think about it. The incubation period for Hep C is 14-180 days. It only takes 1 week for the drugs to wash out of your body (1/128 level) which is below the therapeutic level. By 2 weeks there is only 1/16,348 the level on treatment. So after this time the virus (if there was any left) has, by SVR24 had a full 22 weeks to grow back unimpeded by the effect of the drugs.
It’s logical that if it has not grown back by this stage then the reason is there was nothing left to grow back.
YMMV
If things are settling down and trending better sounds like we can do nothing, with the expectation that will continue.
YMMV
Hi Chris,
Let’s see how you are tomorrow. If you’re worse some antibiotics would be a reasonable idea.
We can sort that out easily enough.
YMMV
Hi Chris,
No this won’t affect your treatment success rate.
In smokers who start coughing up stuff with colour I have a reasonably low threshold for prescribing antibiotics.
Normal smokers cough sputum is white. Viral sputum tends to be yellow and bacterial infection (that will respond to antibiotics) tends to be green(er) but there’s not a lot of visible difference.
The trend is an important thing. You start off well and go downhill. If you keep getting worse that’s a worry, if you stop getting worse and just settle into miserable that’s more ammenable to wait and see.
What country are you in?
YMMV
Hi Chris,
Welcome to the forum. Normal doses of paracetamol or ibuprofen are both fine on DAA treatment.
There is both a flu-like illness (but without the cough and mucus) and a runny nose/sore throat type thing that can happen with DAA treatment.
From what you describe I’d be agreeing with you that you do have something more than just side effects.
What colour is the mucus you’re coughing up?
Do you take any other medications?
Any other medical problems besides the Hep C?
YMMV
Hi Paul,
You have GT3 and cirrhosis (fibroscan > 12.5kPa)
There are no guidelines anywhere in the world that say 8 weeks of Sof+Dac is appropriate for ANYBODY.
The 8 weeks guideline for Harvoni for treatment naive, GT1, Viral load < 6 million, LOW FIBROSIS patients are well known to produce inferior SVR12 to 12 weeks and do not apply to you anyway. You need 24 weeks treatment and would have a high probability of relapse if you do only 8 weeks treatment - nobody knows how high because nobody gives that short a treatment. You should be having ribavirin.
- What country are you in?
- How much longer do you have before you finish the 8 weeks?
- When you do find see your doctor about more treatment?
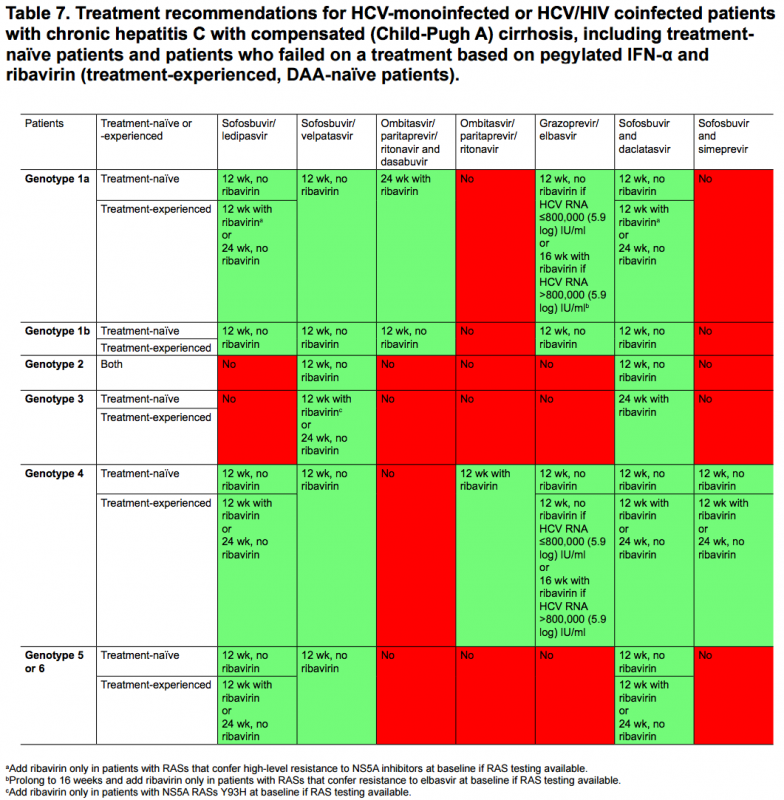
Here are the EASL guidelines for treatment of cirrhotic patients
YMMV
Hello tototo,
With Harvoni 8 weeks is not as good as 12 weeks.
With Mavyret 8 weeks is as good as 12 weeks Harvoni.
It’s possible your stomach bloating and skin itch relate to the Mavyret as rashes and stomach upset are the commonest side effects of any drugs.
I would expect that to settle down when you finish (today!) and that you will achieve SVR12.
YMMV
17 December 2018 at 6:16 am in reply to: REDEMPTION 4 – Epclusa – 12 week course – Experience #28809It is very hard to transmit Hep C without blood to blood contact, so a mother giving it to a child after the bloody events of birth is very rare.
The easiest thing for peace of mind is for you to get treated and SVR12. Check your son one last time at that time. If no antibodies then you have been non-infectious for well over the incubation time and there is no chance your son will come up positive.
YMMV
Hi Jess,
While I can’t promise, and I know you’ll be nervous, for most patients it’s a bit like “am I really taking anything” rather than “these tablets are making me feel sick”.
You can certainly take Zofran if required. I doubt you’ll need it though.
YMMV
Hello MAGA, yes that elevated CK confirms it was related to muscle damage from exercise and the falling AST/ALT are reassuring.
What sort of exercise do you do?
If it is weights you are probably pushing the envelope a bit hard
If it’s endurance then you’re probably not hydrating adequately and overheating
For the blood sugar
<100 is normal
>200 is definitely diabeticAnd between 100-200 is something of a gray area. If you have a look here
http://www.diabetes.org/are-you-at-risk/prediabetes
You will see <100 fasting and <140 following the glucose challenge - so one lab is using the 100 for fasting, the other the 140 for not fasting.
YMMV
Hello kaju,
Your sore tonsils are likely just a cold. The chances of relapse post SVR12 are 1 in 300 – this is very rare, and you are far more likely to be in the 299 than the 1.
Best Regards
James
YMMV
Hi vitrus,
Thanks for your valuable input.
MAGA is a patient of mine who should (theoretically) be straightforward. Reassuringly he feels well, despite the AST/ALT rise.
GT2, low fibrosis (0.7 Fib-4 and 0.559 APRI), Hep B core Ab negative, young(ish) and fit.
We’re getting follow up bloods done to check the trendline on the enzymes and INR to check liver synthetic capacity. Bilirubin has fallen rather than risen.
He takes quite a lot of supplements and exercises extensively so checking CK as the enzymes could be exercise related and stopping the supplements, one of which has a lot of green tea extract (and this has been known to cause liver toxicity problems).
Exercise wise we have seen enzyme rises with kaju https://fixhepc.com/forum/new-to-forum/1748-need-advise-for-gt4-treatment.html?start=45#26349 where the ALT/AST rise appeared to relate to heavy exercise.
I have also seen an acute CMV reactivation mid-treatment but this was associated with significant unwellness and was similar (clinically) to Hep B reactivation.
Anyway we are onto it and are considering if it is a DAA related drug reaction. With any luck the new bloods will show reduced AST/ALT and we can take an expectant approach.
YMMV
We are lucky that all the new medications – Harvoni, Epclusa and Mavyret are remarkably clean in terms of having minimal side effect in most patients. Some people do it harder than others, but overall it’s like chalk and cheese compared to the bad old days of PEG/Riba for 12 months of hell and a 50% chance of cure.
YMMV
-
AuthorPosts
