Forum Replies Created
-
AuthorPosts
-
What genotype are you? Please don’t say 3.
The extra 4 weeks is $500 worth of damn good insurance.
YMMV
Yes this could be a problem for both the Sofosbuvir and the Daclatasvir, both of which would be expected to be at higher levels in your blood stream due to Kratom inhibiting their metabolism. This might be helpful for you as 8 weeks treatment with Sof+Dac for GT1 is borderline – you should take 12 weeks, but is not to be recommended.
https://www.dovepress.com/pharmacokinetics-of-mitragynine-in-man-peer-reviewed-fulltext-article-DDDT
Kratom has the potential herb–drug interaction on cytochrome P450 (CYP) enzyme activity. This was shown in one study, with potent inhibitory effect for CYP3A4 and CYP2D6, moderate effect for CYP1A2, and weak effect for CYP2C19,22 whereas in another study, mitragynine and 7-hydroxymitragynine also showed the inhibitory effect on P-glycoprotein.23 However, there were a few reports of Kratom-related fatalities.
Daclatasvir is metabolised by CYPD3A4 so if you inhibit it with Kratom you will run high levels of Daclatasvir in your blood.
http://www.medscape.com/viewarticle/842315
Sofosbuvir, like many drugs, is partially cleared via the p-glycoprotein transporter (P-GP) system.
So Kratom is also expected to elevate your Sofosbuvir levels and it can be cardiotoxic in high doses.
Advice
You should seriously consider not taking Kratom for the duration of treatment.
You should also seriously consider getting another 4 weeks treatment.
YMMV
Alcohol is not good for your liver, particularly with the added burden of Hep C BUT…..
It will make no difference to whether the treatment works or not. Your odds are as good as anyone else’s, which is pretty damn good.
Here is a piece of research called:
Alcohol Use Among Veterans with HCV Does Not Blunt SVR Rates from DAAs
Or in English – Drinking has no impact on cure rates with the new Hep C drugs.
YMMV
Hi Barry,
Sounds like your indomitable spirit has survived the surgeon’s knife!
YMMV
hydrolysed soya extract inhibited all of the cytochrome P450 isoenzymes tested
So the worst case would be higher levels of Daclatasvir. More sides, but no increased risk of treatment failure.
A good varied diet – not eating the same stuff day after day – is a good way to avoid interactions (known or unknown) as well as being a pretty good way to eat.
YMMV
Hello Teddy,
This is the Antibody test that shows you have been exposed to HepC. There is a 25% chance you have cleared the virus. Was the result you burnt a PCR RNA test?
YMMV
It is not unusual for patients to be a bit tired during the first few days. The way I explain it when discussing what to expect is that it feels a bit like you feel in the days leading up to getting flu. A bit under the weather, but not too bad. This is usually gone within a week or so.
YMMV
If you go here:
http://www.hepatitisc.uw.edu/page/clinical-calculators/apri
You can put in the AST or 27, the upper limit of normal (40) and the platelets of 173 to get an APRI of 0.39.
This is low and the clinical trials often use 2 for cirrhosis.
The high fibroscan probably represents relatively low fibrosis with high inflammation. The inflammation causes swelling and is a bit like blowing up a balloon that is caught in a net. It gets stiff not because there is a lot of net (the fibrosis seen in cirrhosis) but because of the swelling.
I would predict that with treatment AST will end up at 10-15, platelets around 200 and fibroscan drop to 7-9.
What your BF has is at the very mild end of things and a good response is expected.
YMMV
What are his platelets from the full blood count? If > 100 that is good and > 150 that is normal
YMMV
Hello Sonja,
23.4 kPa is > 12.5 kPa which is where we say a patient has cirrhosis.
Yes, this is likely to improve with treatment. I think Hazel here has the record having gone from 40 kPa before treatment to 9.5 kPa after.
These numerical improvements are nice to see but here is what’s really important:
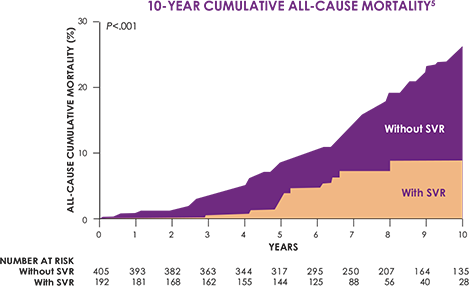
As you can see, patients at SVR are much less likely to die than patients who still have Hep C
YMMV
Hello Akiniai,
If you can find a blood test that says “Hepatitis B surface antibody positive” or a number > 10 (ie not <10) or > 12 then you have protective immunity from Hep B and will not be at risk of reactivation.
YMMV
Hello akiniai,
These results do not provide an answer to the question of whether you do, or do not have chronic Hep B. While you have certainly had Hep B exposure the results you’ve shared don’t answer that question.
What I would need to tell you is Hep B surface antibody. It sounds like you do have that and are immune to Hep B due to prior exposure.
The standard set of blood to answer the question of Hep B status are surface antibody, core antibody, surface antigen as well as some liver function tests.
YMMV
Quercetin INHIBITS CYPD3A4 so can lead to elevation of Daclatasvir levels which is a side effect risk but not a treatment failure risk.
YMMV
Yes, adding Ribavirin now could be of use.
With 4 weeks to go it is possible to get medication to you within that time.
YMMV
Hi Keith,
You have neither NS5A or NS5B resistance. This is good, in fact it does not get any better. 12 weeks Harvoni probably would have done the trick first time round, and would probably still do the trick now.
So really 12-24 weeks of Sof/Led or Sof/Dac or Sof/Vel should all work.
I expect going a little longer than 12 weeks would be good insurance and that skiping Ribavirin would be ok.
We can do (and have done) triple Rx now with available meds but I really don’t think you need it. Would not hurt, but a bit more expensive.
Triples that can be done right now:
Simeprevir+Sof+Dac
Asunaprevir+Sof+Dac
Paritaprevir+Ombitasvir+Sofosbuvir (Viekira+Sofosbuvir)The NS3A components are all originator but come from countries where the prices are much more reasonable.
You could probably use Sof/Vel with Simeprevir or Asunaprevir but I have not looked it up.
YMMV
-
AuthorPosts
