Forum Replies Created
-
AuthorPosts
-
Hello lamussa,
Thanks for the update and congratulations on your SVR12.
My observation is that while Epclusa is a good drug it does seem to have a few more side effects than either Haroni or Sovaldi+Daklinza.
It’s awesome to hear your improvement is sufficient that you don’t need other medications. This is common and one of the nice things about helping people get treated – patients come back and say “Hey, I really do feel better”

YMMV
Hi mrcleanrt,
Congratulations on your result, and…
Hi Ron,
Thank you for the kind words and punching a small hole in the stigma of Hep C by putting your name to it.
With any luck you will see the same sort of fibrosis regression we’ve seen in other patients. Hazel, for example, started at 40kPa and is now down below 8kPa.
It’s a privilege to be able to assist patients to get access to treatment.
Thanks for trying to get the word out. I’m sure you’ve seen the film the Matrix. The deeper you delve into the world of Big Pharma or Big Business the more you realize the world as you think you know it is just a veneer – there are lots of deeper layers…
YMMV
We show your local time to you and my local time to me so the rime you see is the time.
YMMV
Hello Kansuke,
For genotype 2 there is very little difference between Sofosbuvir+Daclatasvir or Sofosbuvir+Velpatasvir.
The Sofosbuvir+Daclatasvir is less expensive and has been around for longer so you might think the more expensive Sofosbuvir+Velpatasvir is better but the reality is there is really not much practical difference.
There are a few reasons to choose one over the other.
For example you can take antacids and Daclatasvir, but you can’t mix antacids and Velpatasvir. For patients with HIV Daclatasvir typically mixes better with the HIV medications, but it depends on the regimen.
Sofosbuvir+Daclatasvir has seem less use in Europe because the $84,000 price for the Sovaldi gets added to the $50,000 for Daklinza making it about twice as expensive as the $74,000 list price for Epclusa. As a generic it’s cheaper, but in originator form it’s more expensive. What this means is that most European doctors will be more familiar with Sof+Vel (Epclusa) so may be happier to prescribe it.
Do you take any other tablets or medications, or have any other health issues?
I’m happy to have a chat with you by video conference and give you a suitable prescription that takes into account price, other medications, etc, etc. You can book at https://gp2u.com.au/
YMMV
Hello Songbird,
You can’t really compare Maviret to Sofosbuvir based regimens and say what is true for the most potent NS3/4A and NS5A agents ever invented is applies to NS5A/NS5B combinations.
HCV represents a heterogeneous quasispecies – the population in any patient exhibits a great deal of variability. It stands to reason some is easy to kill (call them ordinary infantry), some is harder to kill (call them special forces with body armour) and some is harder again to kill (call them tankers).
Rapid viral suppression represents two distinct things. First we are looking at the decline of the easy to kill population (and this is relatively irrelevant) but secondly, and perhaps more importantly, it represents the window period where there are viable replicons and a drug-driven selective pressure on resistance. In the context of drugs being present, we are selecting for the resistant forms to replicate, and one more mutation could be enough to overcome the EC50 of the drugs we are using.
We do know from HIV that continuing to use drugs where the patient has a viral load leads to the development of resistance.
We are lucky that the drugs work as well as they do.
To me, the issue with fibrosis is that the lower blood supply of fibrotic tissue leads to lower tissue concentrations and thus the potential for the drugs to be present at < EC50. The same goes for BMI - we have certainly seen Daclatasvir toxicity in < 50kg patients and treatment failure more common in > 150kg patients. This is a problem with the one size dose fits all model currently in use. Gilead’s research in children adjusts the dose down based on bodyweight (makes perfect sense) but there is no dose adjustment UP for larger people. There is dose adjustment up for many other drugs – antibiotics, anaesthetics, …
YMMV
Hello tototo,
The baseline GT1 cure rate for Maviret is very high. The company says 99% which is probably optimistic but it’s almost certainly as high or higher than Harvoni which is mid-nineties.
So you are GT1a, have previous failure to PEG/Riba (not exactly a failure because you did not do the full course), and are F1/F2, and have HCV RNA <15 but still detected at 4 weeks...
And AFAIK there is no clinical trial that I'm aware of that informs a specific answer for a large group of patients with your specific profile.
Over here you will find an ongoing discussion that would be relative to you if you were taking Harvoni
https://fixhepc.com/forum/questions-and-answers/2064-g3-16-weeks-or-24-weeks.html
And over here you will find an ongoing discussion about how cure rate improves with duration of treatment
https://fixhepc.com/forum/experts-corner/2062-shorter-time-for-treatment.html
Questions: how long are you scheduled for, and how good is your insurance?
If you're scheduled for 8 weeks your SVR12 probability has probably fallen from high 90s to lower 90s
If you have good insurance then retreatment for longer with Maviret+Sof or Vosevii will have a mid 90s probability of success so it's not the end of the world if the first treatment does not work (and the odds are still very much that it WILL)
YMMV
Hello Songbird,
This study was published in 2015 and the conclusions came from pooled data from small clinical trials.
Here’s a much larger VA study 4,365 patients all taking Harvoni that followed this and was published April 2016.
pp408
Significantly lower SVR rates were observed in those receiving LDV/SOF who had a 4-week on-treatment detectable HCV RNA <15 IU/mL compared to those who were undetectable by week 4.
pp410
Four-week on-treatment HCV RNA was an independent predictor of SVR when included as a variable in the models (Supporting Table S2). Having a detectable HCV RNA <15 IU/mL was associated with reduced odds of SVR compared to undetectable in the full model (OR 0.40, 95% CI 0.29-0.56, P<0.001)and in the model limited to those who completed 12weeks of treatment (OR 0.38, 95% CI 0.25-0.58, P<0.001).
pp413
In this analysis, 4‐week viral kinetics predicted SVR with a greater effect in those who received LDV/SOF. Significant reductions of 10.5% and 7.1% in SVR rates were observed in patients receiving LDV/SOF and LDV/SOF+RBV, respectively, who had a detectable 4‐week HCV RNA ≥15 IU/mL compared to those with undetectable 4‐week HCV RNA. In patients who completed 12‐week courses of LDV/SOV there remained a significant 6.4% reduction in SVR rates between those with detectable 4‐week HCV RNA ≥15 IU/mL and those with undetectable 4‐week HCV. For those who completed 12 weeks of LDV/SOF+RBV the difference in SVR rates was no longer statistically significant. In multivariable analysis, having a HCV RNA ≥15 IU/mL after 4 weeks of treatment was associated with a 60% reduced odds of achieving SVR for the cohort and a 62% reduced odds of achieving SVR for those who completed 12 weeks of treatment. The VA guidance recommends obtaining 4‐week HCV RNA testing, thus providing a large sample size to evaluate this variable which has not generally been assessed in prior LDV/SOF studies. The clinical implications of this finding on treatment decisions, such as potentially adding RBV or extending treatment duration based on 4‐week on‐treatment HCV RNA, warrant further study.
Call it an inconvenient truth if you like, but a truth it is. I have 3460 patients at last count and initial slow responders used to feature disproportionately in the retreatment group. They feature less now because I extend or modify their treatment.
You may find this interesting in terms of digging into the science of what needs to be done to get to cure:
https://www.bhiva.org/file/lOvBacnRQiHzM/ValeriaCento.pdf
You may also note that this is an early study based on small numbers and concludes in a 1/2 and 1/2 way saying
- In contrast with IFN-containing regimens, a Rapid Viral Response after 4 weeks of INF-free treatment seems not to correlate with SVR12 (proven wrong by VA)
- Cirrhotic patients have a slower HCV-RNA kinetics, and in this population response-guided therapy can still have a role in determining the optimal duration of treatment. (right)
YMMV
This is a <15 result but still detected. It is a good result at 21 days and your liver engymes are great. Your urea levels depend on how much you drink, yours is low and this just means you drink a bit more water than average.
For most people who are treatment naive and low fibrosis 8 weeks of Maviret is enough. The doctor who prescribed it would be the best person to ask as I don't know your full background and history.
YMMV
Hello Songbird,
I’m not talking about EOT results. I’m talking about on treatment kinetic decay, or more specifically rate of kinetic decay.
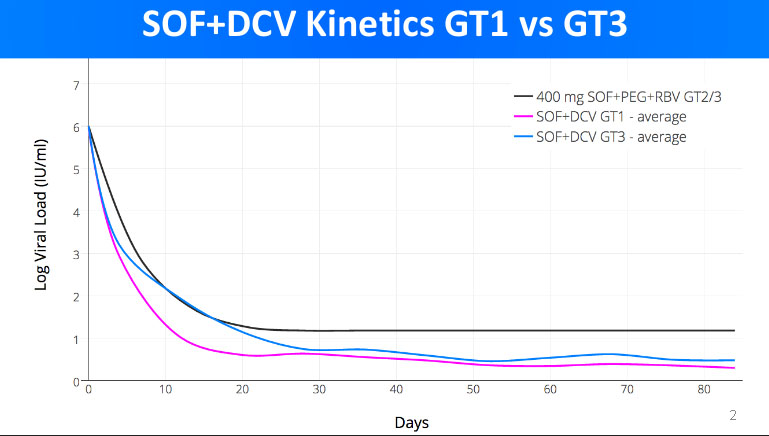
If you have a look here https://fixhepc.com/component/k2/itemlist/tag/International%20Liver%20Congress%202016.html you will see my original presentation to EASL in 2016. It contains 2 graphs about the kinetic decay of the viral load. The first is a comparator to SOF+PEG+RIBA to SOF+LDV and SOF+DCV. The
At the time I had some unique data, namely the kinetic decay for SOF+DCV in patients with both GT1 and GT3 as well as SOF+LDV for GT1. The upshot is that SOF+DCV produces a slightly faster kinetic decay than SOF+LDV in GT1 patients, and that, for SOF+DCV the GT3 kinetic decay is considerably slower than GT1.
The significance of the rate of kinetic decay is that logically we need to get to ~0-100 total virions left to get cure. This is the infective dose and also way too small to measure as you have 1000 5ml tubes of blood in you so even if the virus was completely blood born, and the cure remainder was <100 viruses only 1 in 10 blood tubes would have a single virus in it.
Anyway, it follows that if you are going down slower you need to treat for longer to have the same overtreatment insurance buffer.
YMMV
Hello Elizabeth,
Without knowing the exact details it’s hard to give proper advice but…
- We know that GT3 is hardest to cure, particularly in the context of having cirrhosis
- We can observe your doctor was sufficiently concerned to add ribavirin
- We know that about 22% of patient will detected at 4 weeks, and also that these people form 44% (our data) or 50% (US VA data) of the treatment failures
- Being still detected at 12 weeks is, therefore, a worry
- The generic retreatment options for GT3 are severely limited, so
- Given we know that longer treatment is more effective than shorter treatment, if you have the ability to treat for 24 weeks, and this is affordable, and your mother is travelling OK on the treatment, I would definitely suggest you do a full 24 weeks.
PS: If you have to pay for the PCR I would suggest saving that money (it adds nothing to the cure rate) and spending it on more medication to extend the treatment duration. While showing up undetected is nice, it is pretty meaningless in terms of treatment decisions ie treat for longer or not. You mother has responded slowly so has pretty resistant virus.
YMMV
Hello tototo,
It is almost certainly a drug allergy.
Some patients with liver disease get itchy due to the build up of toxic stuff. These people generally get better with treatment.
With any drug, stomach upsets and rashes are the two commonest side effects.
In terms of treatment success it’s neither a good or a bad sign, unless it means you can’t complete your full treatment. The options are:
1) Stop the medications (and you will probably relapse)
2) Take an antihistamine like Claratyne (loratidine), Zertec (cetirazine) Phenergan (promethazine) which may help settle it down – for other antihistamines check interactions at https://www.hep-druginteractions.org/checker (but these 3 are all fine with Maviret)
3) Get hold of some generic Epclusa and swap over to taking that to get the treatment duration out to 12 weeks.Attachments:
YMMV
Hello tototo,
For any of the DAA medications the cure rate looks like this:
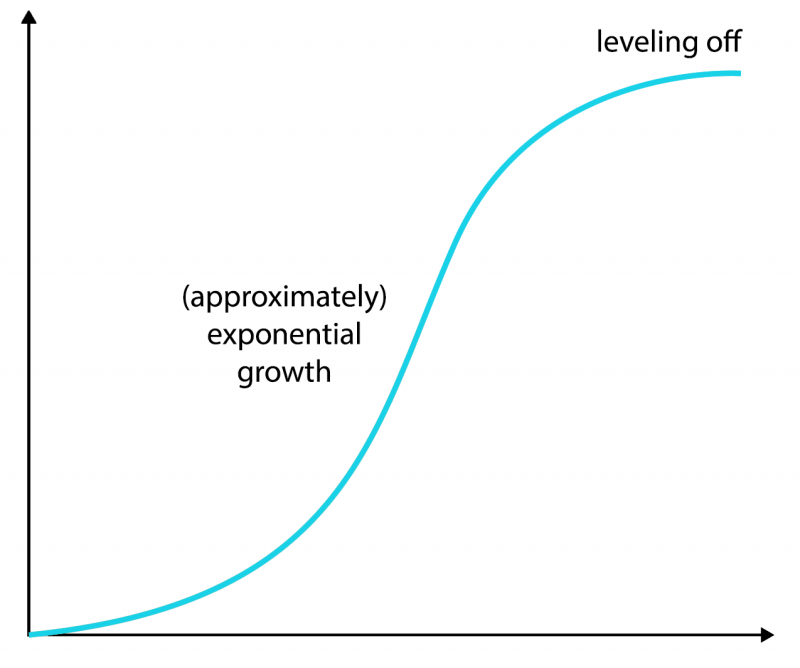
Below 4 weeks there is virtually no cure rate. This relates to the 1/2 life of the replicon being around 4 weeks so you need to “keep killing” it for at least this long otherwise it will recover.
Then on the far right you see the reality. Every extra week of treatment adds a little more to the cure rate, but each extra week adds less than the previous one.
We know that for any patient who is cured we were giving them drugs for at least one day, maybe one week, maybe one month too long but we have to strike a balance between cure rate and duration and our tests are not sensitive enough to detect cure.
For Harvoni the cure rate @ 8 weeks is ~90% and 12 weeks is 95% – that’s from the VA data not the Gilead company data. Most of our retreatment cases got only 8 weeks Harvoni.
Maviret is good and the 8 week treatment should give you a ~95% chance of cure. Longer would be nice but you probably just have to chance it at this stage as at day 24 you’re almost 1/2 way through. The odds are 20:1 in your favour.
YMMV
Hello MAGA,
Welcome to the forum. Best of luck with the treatment. It can be a bit lonely but there is really good support here from people who have walked the exact same road.
YMMV
-
AuthorPosts
